For millions of people worldwide, gastroesophageal reflux disease (GERD) turns nighttime into a battleground. The burning sensation creeping up the chest, the sour taste in the mouth, and the interrupted sleep create a vicious cycle that impacts overall well-being. While medications and dietary changes play crucial roles in management, one often overlooked aspect is sleep positioning. The way we position our bodies during sleep can significantly influence the frequency and severity of acid reflux episodes.
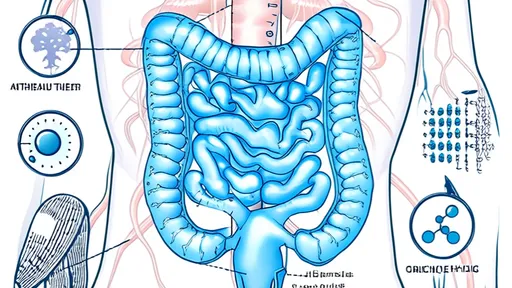
The relationship between sleep posture and GERD symptoms isn’t merely anecdotal—it’s grounded in anatomy and physics. When lying flat, gravity ceases to assist in keeping stomach acids where they belong. This allows acidic contents to more easily breach the lower esophageal sphincter (LES), the valve-like muscle separating the stomach from the esophagus. Over time, repeated exposure to stomach acid can damage esophageal tissue and exacerbate symptoms. This is why understanding optimal sleep positions becomes not just about comfort, but about protecting one’s health.
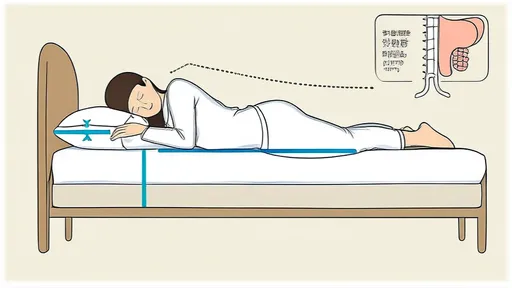
Elevating the upper body emerges as a cornerstone strategy for reflux sufferers. Studies have shown that raising the head of the bed by approximately six to eight inches creates a gentle incline that helps prevent stomach acid from traveling upward. This elevation doesn’t require dramatic changes to one’s sleeping environment—special wedge pillows designed for GERD patients or simple bed risers placed under the headboard legs can achieve the desired effect. The key lies in creating a smooth incline rather than propping up with multiple pillows, which can actually worsen reflux by bending the body at the waist and increasing abdominal pressure.
The left-side sleeping position has gained particular attention in gastroenterology circles. This preference stems from the stomach’s natural anatomy—when lying on the left side, the stomach sits below the esophagus, making it more difficult for acid to escape upward. Some research suggests this position may also promote faster gastric emptying. Many patients report noticeable improvement in nighttime symptoms after consistently adopting left-side sleeping, though the transition may feel unnatural initially for those accustomed to other positions.
Conversely, right-side sleeping tends to be the worst offender for reflux sufferers. In this position, the stomach sits above the esophagus, essentially providing a direct path for acid to travel upward. The difference between left and right-side sleeping can be so pronounced that some patients find they can prevent nighttime awakening simply by training themselves to avoid the right-side position. This dramatic positional effect explains why some people experience reflux even when following all other dietary and medical recommendations perfectly.
Back sleeping presents a mixed scenario for GERD patients. While preferable to right-side sleeping, the supine position still allows acid to pool more easily than left-side sleeping. For those who cannot comfortably sleep on their side, combining back sleeping with proper upper body elevation becomes crucial. Some patients find additional relief by placing a small pillow under their knees, which helps maintain spinal alignment while preventing the sliding down that can occur with elevated head positions.
Stomach sleeping generally ranks as the most problematic position for acid reflux sufferers. The prone position puts direct pressure on the abdomen, increasing intra-abdominal pressure that can force stomach contents upward. Additionally, the neck rotation required for breathing in this position can create musculoskeletal issues over time. While it may be challenging for lifelong stomach sleepers to change habits, the potential reduction in nighttime symptoms often provides sufficient motivation to transition to more reflux-friendly positions.
The journey to finding the optimal sleep position for GERD management often requires patience and experimentation. Some patients benefit from positional training aids like body pillows that prevent rolling onto the back or right side during sleep. Others find that combining positional changes with timing of meals—avoiding food within three hours of bedtime—creates a synergistic effect. The gradual nature of improvement means consistency matters more than perfection; even partial adherence to better sleep positions can yield noticeable benefits over time.
Beyond immediate symptom relief, proper sleep positioning may contribute to long-term esophageal health. By reducing the frequency and duration of acid exposure to esophageal tissue, patients may lower their risk of developing complications like esophagitis or Barrett’s esophagus. This preventive aspect makes sleep positioning not just a comfort measure, but potentially a protective strategy against disease progression.
Individual variability means there’s no one-size-fits-all solution to sleep positioning for GERD. Factors like body shape, presence of hiatal hernia, and severity of LES dysfunction all influence how dramatically positional changes affect symptoms. Some patients may require combination approaches—using elevation alongside left-side sleeping—while others find one modification sufficient. Working with a gastroenterologist can help tailor these general recommendations to individual circumstances.
The interplay between sleep quality and GERD creates a complex feedback loop. Poor sleep exacerbates stress and inflammation, which may in turn worsen reflux symptoms. By improving sleep through positional adjustments, patients may experience secondary benefits in their overall GERD management. This holistic impact underscores why sleep positioning deserves attention equal to other lifestyle modifications in reflux treatment plans.
Implementing these changes requires more than just understanding the concepts—it demands practical solutions that fit into real lives. For couples sharing a bed, compromise may be necessary to accommodate one partner’s need for elevation or side sleeping. Temperature-regulating mattress toppers can help address the increased warmth some experience with wedge pillows. The market has responded to these needs with innovative products ranging from adjustable beds to smart pillows that gently vibrate when detecting unfavorable sleep positions.
Measuring progress remains an important part of the process. Patients might keep a sleep diary tracking positions, elevation use, and symptom severity to identify what works best. Over weeks and months, patterns emerge that can guide fine-tuning of the approach. Celebrating small victories—like consecutive nights without awakening to acid reflux—helps maintain motivation through the adjustment period.
As research continues to evolve, the connection between sleep dynamics and digestive health reveals increasing complexity. Emerging studies explore how different sleep stages affect LES pressure and gastric emptying rates. This growing body of knowledge promises more personalized approaches to sleep positioning in the future, potentially identifying subgroups of patients who might benefit from specific variations on these general recommendations.
For now, the evidence strongly supports sleep position adjustment as a valuable, low-risk intervention in GERD management. Unlike medications that may carry side effects or dietary changes that require significant lifestyle alterations, positional therapy offers a simple yet effective tool. By working with the body’s natural anatomy rather than against it, patients can reclaim restful nights and reduce their dependence on other interventions. In the comprehensive management of acid reflux, sometimes the most powerful solutions lie in how we position ourselves when we’re most vulnerable—during sleep.

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025