The silent thief of bone density often goes unnoticed until the first fracture occurs. Osteoporosis, a condition characterized by weakened bones prone to fractures, affects millions worldwide, particularly postmenopausal women and older adults. While medical professionals use advanced tools like DEXA scans for diagnosis, simple self-assessment questionnaires can serve as valuable early warning systems. These accessible screening tools help individuals recognize potential risk factors and seek timely medical intervention.
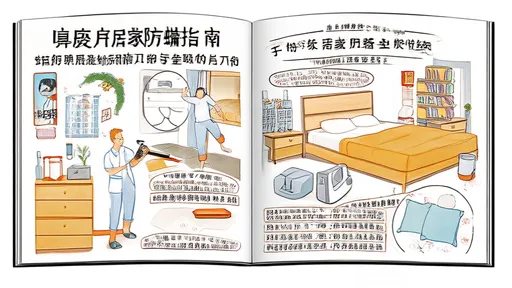
Understanding the importance of bone health assessment begins with recognizing osteoporosis' insidious nature. Unlike many health conditions that present obvious symptoms, bone density loss typically progresses without pain or visible signs. Many individuals remain unaware of their deteriorating bone health until suffering a fragility fracture from minor bumps or falls. This makes proactive risk assessment crucial, especially for those in high-risk categories. A well-designed 10-question self-test can highlight risk factors ranging from family history to lifestyle choices that may contribute to bone mineral density loss.
The foundation of any effective osteoporosis risk questionnaire lies in its ability to identify both modifiable and non-modifiable risk factors. Non-modifiable elements include age, gender, family history of osteoporosis, and personal history of fractures. Women over 50, particularly those who have experienced early menopause, face significantly higher risks. Similarly, individuals with a parent who suffered a hip fracture demonstrate greater predisposition to bone density issues. These immutable factors help establish baseline risk levels that determine how aggressively one should pursue preventive measures.
Lifestyle factors constitute the other critical component of osteoporosis risk assessment. Dietary calcium and vitamin D intake, physical activity levels, smoking status, and alcohol consumption all profoundly impact bone health. Many self-assessment tools inquire about dairy product consumption or supplement use, as inadequate calcium intake remains a widespread issue. Sedentary behavior emerges as another red flag, as bones require regular weight-bearing exercise to maintain their density. Questions about tobacco and alcohol use help identify additional reversible risk factors that individuals can address to improve their bone health outlook.
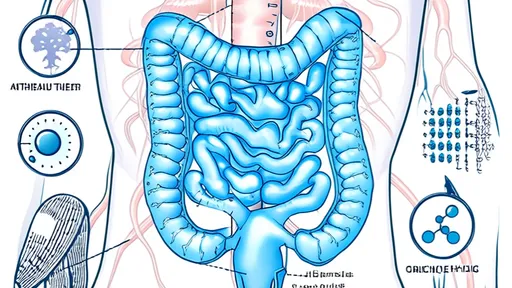
Certain medical conditions and medications warrant special attention in osteoporosis risk evaluation. Rheumatoid arthritis, celiac disease, hyperthyroidism, and chronic kidney disease all associate with increased bone loss. Similarly, long-term use of corticosteroids, some anticonvulsants, and proton pump inhibitors may compromise bone density. A comprehensive self-assessment should include questions about these conditions and medications, as they might necessitate earlier or more frequent professional bone density testing.
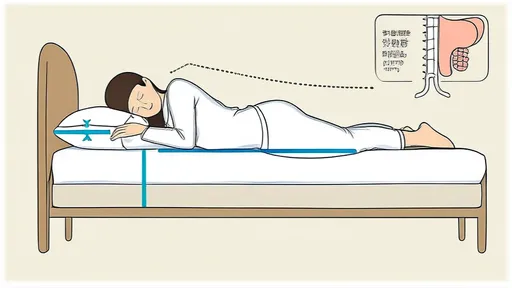
Body composition metrics like height and weight provide simple yet revealing indicators of osteoporosis risk. Significant height loss in adulthood often signals vertebral compression fractures, while low body weight (particularly a BMI under 19) correlates with reduced bone density. Many self-assessment tools include questions about noticeable height reduction or difficulty reaching high shelves, which may indicate spinal changes. These physical changes frequently go unnoticed in daily life but serve as important warning signs when properly assessed.
The predictive power of osteoporosis risk questionnaires lies in their ability to synthesize multiple risk factors into an overall risk profile. While no single "yes" answer definitively indicates osteoporosis, accumulating several risk factors significantly increases the likelihood of bone density issues. This cumulative risk approach helps individuals understand how various aspects of their health and lifestyle interact to affect their skeletal strength. It also provides motivation for making positive changes, as addressing even a few modifiable risk factors can substantially improve bone health outcomes.
Interpreting self-assessment results requires understanding that these tools serve as screening instruments rather than diagnostic tests. A high-risk score doesn't confirm osteoporosis but indicates the need for professional evaluation. Conversely, a low-risk score doesn't guarantee perfect bone health, especially if new risk factors emerge later. The most valuable outcome of such self-assessment is prompting timely conversations with healthcare providers about bone density testing and preventive strategies tailored to individual risk profiles.
Implementing changes based on risk assessment findings can dramatically alter one's bone health trajectory. Increasing dietary calcium, starting vitamin D supplementation, beginning weight-bearing exercises, or quitting smoking all represent concrete actions that strengthen bones. For those at highest risk, medical interventions like bisphosphonates or hormone therapy might become considerations. The self-assessment process empowers individuals to take proactive steps rather than waiting for fractures to occur before addressing bone health concerns.
Regular reassessment forms the final piece of effective osteoporosis risk management. As age advances and health circumstances change, so too does osteoporosis risk. Repeating the self-assessment annually or when experiencing significant health changes (like new medications or diagnoses) ensures ongoing awareness of bone health status. This longitudinal approach allows for early detection of emerging risk factors and timely adjustment of prevention strategies, maintaining skeletal strength through all life stages.
The accessibility and simplicity of osteoporosis risk self-assessments make them powerful tools for public health. By raising awareness and encouraging early intervention, these questionnaires can reduce the substantial personal and economic costs associated with osteoporotic fractures. While not replacing medical evaluation, they serve as important first steps in preserving mobility, independence, and quality of life as we age. Taking ten minutes to complete such an assessment today might prevent years of disability tomorrow.

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025