For millions of individuals managing hypertension, the first moments after waking can set the tone for the entire day. Emerging research suggests that specific morning movements and postural adjustments may significantly impact blood pressure regulation. This article explores the science behind optimal morning routines for hypertensive patients, offering practical guidance grounded in current medical understanding.
The Physiology of Morning Blood Pressure Surges
Circadian rhythms create natural fluctuations in blood pressure throughout the day, with the most dramatic spike typically occurring during the early morning hours. This phenomenon, known as morning surge, results from complex interactions between the sympathetic nervous system and hormonal changes. Cortisol levels peak around wake-up time, while the body transitions from parasympathetic to sympathetic dominance. For hypertensive individuals, this biological process can create dangerous cardiovascular strain if not managed properly.
Medical imaging studies reveal that blood vessels demonstrate reduced elasticity during these morning hours. The endothelium—the inner lining of arteries—appears particularly vulnerable to damage when subjected to sudden pressure changes upon waking. This explains why cardiovascular events show marked temporal patterns, with heart attacks and strokes occurring most frequently between 6:00 AM and noon.
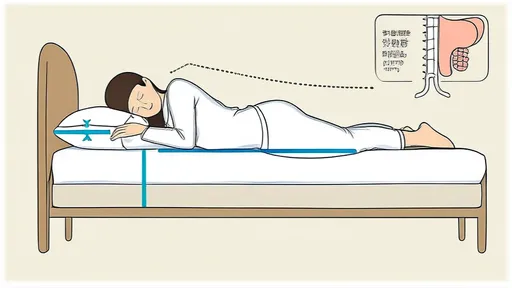
Transitioning from Sleep to Wakefulness
The act of rising from bed requires careful consideration for hypertension patients. Abruptly sitting upright creates immediate orthostatic stress as the cardiovascular system adapts to positional changes. Specialists recommend a gradual three-stage process: beginning with brief wakeful lying, progressing to seated edge-of-bed positioning, and finally achieving standing posture. This phased approach allows baroreceptors—pressure sensors in major arteries—to properly adjust to gravitational changes.
During the initial wakeful lying phase, simple isometric exercises prove beneficial. Gentle ankle circles and wrist rotations stimulate venous return without dramatically elevating heart rate. These subtle movements prepare the circulatory system for more significant activity while maintaining stable blood pressure parameters. Patients often overlook this critical transition period, yet it serves as the foundation for safer morning mobility.
Postural Considerations and Movement Mechanics
Proper body mechanics during the rising process significantly influence cardiovascular response. The standard recommendation involves using arm support to push upright rather than relying solely on abdominal muscles. This technique reduces intra-abdominal pressure that could otherwise translate to vascular strain. When moving from sitting to standing, maintaining slight knee flexion helps distribute the postural load across multiple muscle groups rather than concentrating demand on the cardiovascular system.
Balance plays an often-underestimated role in blood pressure management. Instability during standing triggers adrenaline release as the body attempts to prevent falls—this catecholamine surge directly impacts blood pressure. Simple balance exercises performed while seated on the bed edge, such as heel-toe rocking or single-leg lifts, enhance proprioception and reduce the need for compensatory cardiovascular responses during upright transitions.
Breath Control Techniques
Respiratory patterns profoundly influence morning blood pressure dynamics. The Valsalva maneuver—inadvertently performed when holding breath during movement—creates dangerous pressure spikes. Conscious diaphragmatic breathing should accompany all transitional movements. A recommended pattern involves inhaling during preparation phases and exhaling during exertion phases of movement.
Advanced techniques incorporate paced breathing with specific ratios. The 4-7-8 method (inhale for 4 counts, hold for 7, exhale for 8) has demonstrated particular efficacy in blunting morning blood pressure surges when practiced during wake-up routines. This controlled breathing not only manages immediate pressure responses but also establishes parasympathetic tone that carries through the morning hours.
Environmental Factors and Morning Preparation
Bedroom conditions significantly impact these morning cardiovascular transitions. Ambient temperature deserves special attention—cool environments trigger vasoconstriction while excessive warmth promotes dehydration. Maintaining a neutral thermal zone helps prevent unnecessary vascular stress. Hydration status from overnight significantly affects morning blood viscosity; keeping water bedside for small sips upon waking can improve circulatory dynamics.
The timing of morning medications interacts crucially with movement protocols. Some antihypertensives require specific positioning for optimal absorption, while others need time to reach therapeutic levels before physical activity. Consultation with prescribing physicians can help synchronize pharmaceutical and movement strategies for maximal morning protection.
Long-Term Adaptation and Progress Monitoring
Implementing these morning movement protocols creates measurable physiological adaptations over time. Baroreceptor sensitivity improves with consistent practice, leading to more stable transition periods. Patients should track morning blood pressure at multiple time points—immediately upon waking, after positional changes, and following morning routines—to identify patterns and refine their approach.
Technological advances now enable sophisticated monitoring of these morning transitions. Wearable devices can track heart rate variability during wake-up sequences, providing feedback for protocol optimization. This biofeedback approach allows for personalized refinement of morning movement strategies based on individual physiological responses rather than generic recommendations.
The cumulative effect of proper morning movement protocols extends far beyond the wake-up period. By establishing stable cardiovascular parameters early in the day, patients often experience more controlled blood pressure patterns throughout waking hours. This comprehensive approach represents an often-overlooked yet critical component of hypertension management—one that bridges pharmaceutical treatment and lifestyle modification for optimal results.

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025